Maximize Claims Success
Premier RCM services for scaling DSOs
- Increase practice profits
- Reduce administrative burden
- Save staff time
Trusted By Leading DSOs








The Complete Verification Solution for DSOs
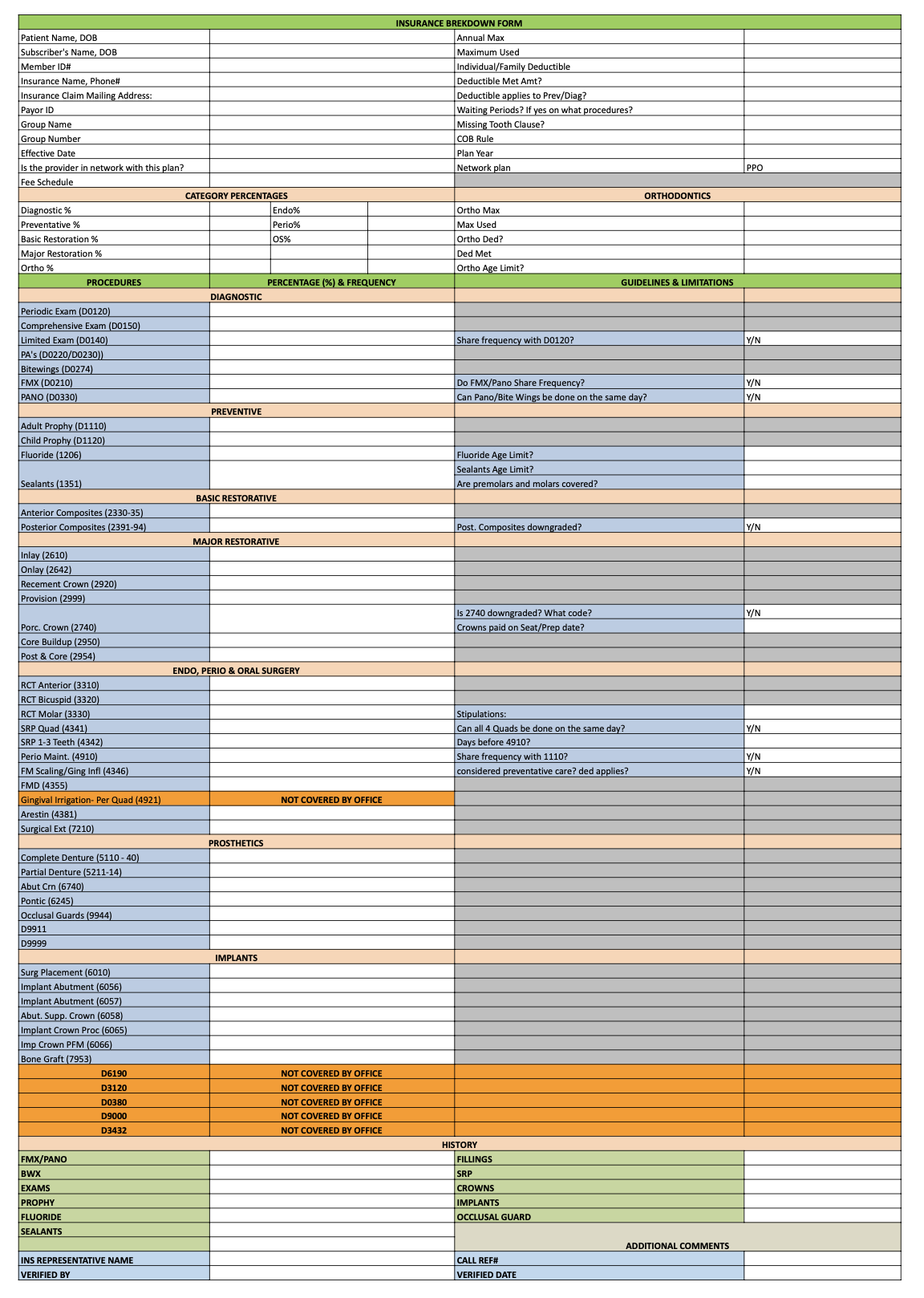
Move from errorprone and burdensome verifications to Dntel's end-to-end, fully customized and filled out verifications.
End-to-End Service
PMS reading, fully completed + customized breakdowns, and full writebacks into any PMS. Handles per location SOPs and complex cases like umbrella networks.
AI+Human Excellence
Veteran verification experts are combined with best-in-class AI payer portal and calling agents to deliver unmatched accuracy and efficiency.
Full Visibility
A single dashboard providing real-time visibility and error handling, complete with per-location controls and reporting. Save time with features like auto-2FA capturing.
Quantifiable Results
Save time, money, operational burden, and denials with Dntel.
Cheaper
Significantly lower costs compared to in-house verification teams.
Minutes Saved Per Patient
Completely remove the need for gathering verification information.
Audited Verifications
All forms are audited ensuring clean claims and fewer denials.
Impact for a Typical 100-Location DSO Per Year
Customized Breakdowns for Every Location
Dntel allows for arbitrary customized breakdowns across any subset of locations to handle each location's unique needs.
Key Benefits
- Support for arbitrary codes, limitations, and exclusions
- Not restricted to information only on payer EDI's or portals
- Configurable location specific benefit rules and SOPs saved
- Editable group templates usable year over year
- Easy editing ability to add or delete fields as needed
How Dntel Compares
See why customers are switching to Dntel no matter their current verifications process.
Dntel vs. Software
Existing software-only providers provide a fraction of available insurance info, forcing internal staff to still wait on hold and call payers or look up payer portals, which can still be > 30 min / verification.
Dntel provides complete info by looking at all sources, removing the need for staff to do any verifications.
Dntel vs. In-House
In-house are great but are 4x more expensive than Dntel and create a much larger operational footprint.
Dntel removes the need for individual verification reps while integrating cleanly with front-office staff and RCM leaders.
Dntel vs. Outsourced
Dntel's AI-powered workforce provide more accurate and faster results.
Dntel's dashboard and experience such as auto-capturing 2FA codes, reduces front-office distraction and enhances overall real-time RCM visibility + process optimization.
Simple Onboarding Process
Onboarding to 100+ locations is seamless and can be done in 2-3 months.
Single Location Pilot
- Dntel receives custom verification form from office
- Dntel provides sample form fills and write backs for office to QA quality of results for a set of patients across different payers
Single Location Onboarding
- Office staff and DSO RCM leaders receive dashboard logins and access
- Dntel spends ~2 weeks providing end-to-end verification services
Multi-Location Scale
- Dntel onboards the rest of the locations iteratively, setting up location-specific verification forms as needed and login credentials
- DSO RCM leaders can monitor everything on their dashboard
Clean verifications lead to clean claims.
Are you ready to take control of your denials?
Schedule a Demo